
The most common symptom of endometriosis is pelvic pain. This information can help your health care provider make diagnosis and treatment decisions. Include details about what factors increase or decrease the symptoms and in what ways they affect your lifestyle. Write down when and where you have pain or other symptoms of endometriosis.
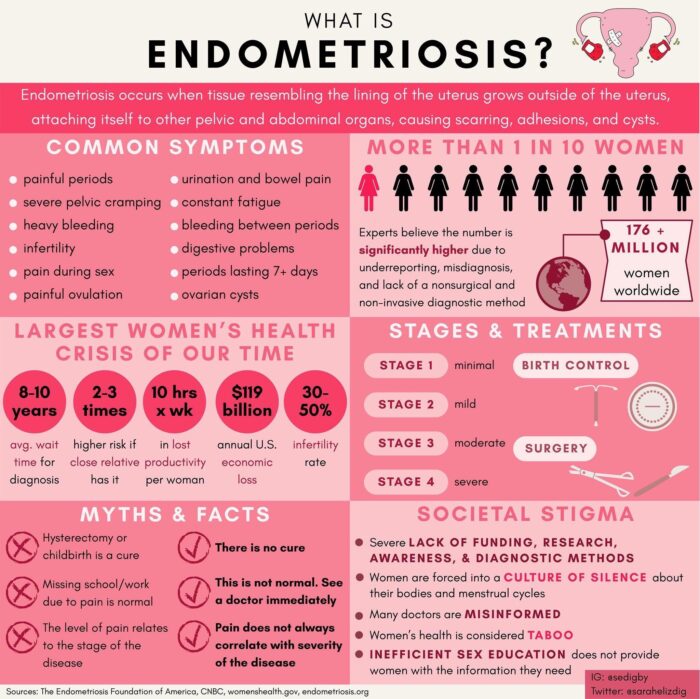
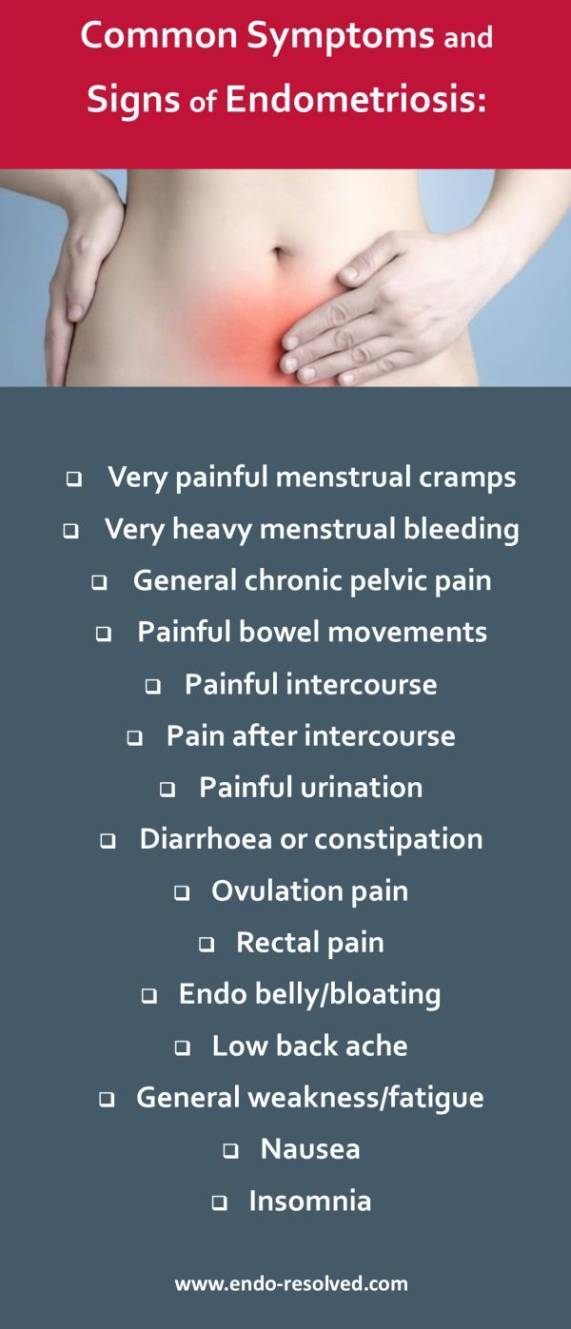
Many conditions, other than endometriosis, can cause pelvic pain, including internal scarring, chronic appendicitis, irritable bowel syndrome, interstitial cystitis and hernias, as well as endometriosis. Pelvic pain can mean many different things.ĭaily pelvic pain may be a sign of problems with your bladder, bowels, reproductive organs or pelvic muscles. But for other women, the pain associated with endometriosis can lead to fatigue, feelings of depression and isolation, problems with sex and relationships, and difficulty fulfilling work and social commitments. In fact, some women with endometriosis may not experience any symptoms at all, and will never be aware they have the disease. The symptoms are different for every woman. Some women have very little endometriosis but lots of pain and others have severe endometriosis with no pain. Patients presenting with minimal disease may have debilitating pain, whereas other clients with severe stage III–IV disease are asymptomatic (Hsu et al., 2010).Generally, the symptoms you experience will depend on where your endometriosis is located and how extensive the growth is however, there is not always a direct correlation between the extent of the disease and the symptoms. Interestingly, the objective signs and subjective symptoms associated with pelvic pain do not always correlate.
Chronic pelvic pain (> 6 months, most common sx).Determining diagnosis based soley on clinical presentation is challenging due to the wide range of symptoms, which can often overlap with several other gynecologic and nongynecologic conditions, including chronic pelvic inflammatory disease and irritable bowel disease (Mao & Anastasi, 2010). The clinical presentation of endometriosis varies greatly in severity, symptoms, and impact on the physical, social, and mental health of the woman. Altered immunosurveillance: endometriosis occurs either when the immune system is overwhelmed by menstrual back flow, or when a defective system allows the lesions to escape immunosurveillance, establish a blood supply, and continue to thrive.However, this theory does not account for gravity-dependent locations of implants, which constitute the majority of distant endometriotic implants (Bloski & Pierson, 2008). This could explain how endometriotic implants migrate to locations such as lungs, bone, and skin. Vascular and lymphatic spread: endometrial tissue infiltrates the local blood supply and lymphatic systems, and subsequently travels to distant sites in the body.Celomic metaplasia: celomic cells, which differentiate from peritoneal cells, become endometrial cells that respond to triggers such as menses, toxins, or immune factors in a cyclic manner (Mao & Anastasi, 2010).While widely accepted, this cannot be the sole cause of endometriosis because a majority of women experience some degree of retrograde menstruation, however few develop endometriosis (Mao & Anastasi, 2010).

This is the portion of the uterus that changes throughout the menstrual cycle, becoming thick and rich with blood vessels to prepare for pregnancy, then shedding if the woman does not become pregnant (Burney & Giudice, 2012).Įndometriosis is defined as the presence of endometrial glands and stroma in ectopic locations, or locations other than the interior of the uterus. The endometrium is the mucous membrane layer that lines the inside of a female’s uterus.


 0 kommentar(er)
0 kommentar(er)
